You may have heard the terms ‘Medi-Cal’ and ‘Covered California’ be used in discussions regarding health coverage. Understanding the differences between these two programs is important to make an informed decision about health coverage for you and your family.
Medi-Cal
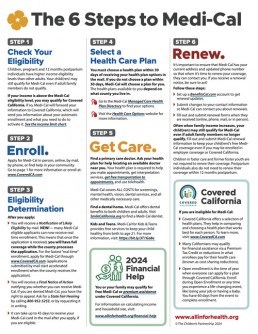
Medi-Cal is a public health insurance program available to low-income Californians. Starting January 1, 2024, all income-eligible Californians qualify for full scope Medi-Cal benefits REGARDLESS OF AGE OR IMMIGRATION STATUS. Full scope Medi-Cal covers more than just care when you have an emergency. It provides medical, dental, mental health, and vision (eye) care. Applying for Medi-Cal via the Covered California website is the fastest way to get covered.

Covered California
Covered California is a free service for individuals and families to get free or low-cost health insurance OR to get help paying for private health insurance services, prescription drugs, and more.
Medi-Cal covers vital health care services for you and your family, including doctor visits, prescriptions, vaccinations, mental health care, and more. So, if you have Medi-Cal, make sure you renew it when it’s time.
Annual Medi-Cal renewals began in April 2023. Renewals are usually due in the same month you first enrolled in Medi-Cal. For example, if you first enrolled in May 2023 you will need to renew in May of 2024.
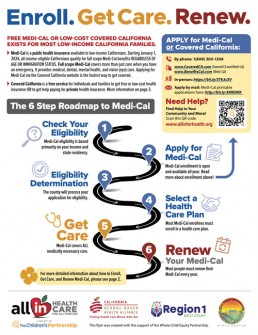
6 Steps to Enroll, Get Care, and Renew your Medi-Cal:
*You can also find these steps in our Health Coverage fact sheet, which you can download above
Step 1: Check your eligibility
- Medi-Cal eligibility is based primarily on your income and state residency.
- Children, pregnant and 12 months postpartum individuals have higher income eligibility levels than other adults. Your child(ren) may still qualify for Medi-Cal even if adult family members do not qualify.
- Check the income chart to see if you or your family qualifies
Step 2: Enroll
- Apply for Medi-Cal:
- In person: https://bit.ly/3Tk3cXV
- Online:
- http://www.CoveredCA.com (Covered CA and Medi-Cal)
- www.BenefitsCal.com (Medi-Cal)
- By mail: Medi-Cal printable applications here: http://bit.ly/3RRENIK
- By phone: 1(800) 300-1506
Step 3: Eligibility Determination
- The county will process your application for eligibility.
Step 4: Select a Health Care Plan
- You must choose a health plan within 30 days of receiving your health plan options in the mail. If you do not choose a plan within 30 days, Medi-Cal will choose a plan for you. The health plans available to you depend on what county you live in.
Step 5: Get Care
- Find a primary care doctor. Ask your health plan for help locating an available doctor near you. Your health plan is required to help you make appointments, get interpretation services, get free transportation to appointments, and use telehealth.
Step 6: Renew!
- It’s important to ensure that Medi-Cal has your current address and updated phone number so that when it’s time to renew your coverage, they can contact you. If you receive a renewal notice, be sure to act!
- Set up a BenefitsCal.com account to get renewal updates.
- Submit changes to your contact information so Medi-Cal can contact you about renewals. You can contact your county Medi-Cal office, by mail, phone, or in person. To find your county Medi-Cal office, visit dhcs.ca.gov/COL or call (800) 541-5555.
- Fill out and submit renewal forms when they are received (online, phone, mail, or in person).
NEED HELP? If you need assistance with your Medi-Cal renewal, call the Medi-Cal Member Helpline at (800) 541-5555 or find help in your community at allinforhealth.org/get-help.

Children, teens, and young adults (under age 21) qualify for free services and support to stay or get healthy. These services include check-ups, shots, and health screenings. Also included are treatments for physical, mental, and dental health problems.
Schedule a Free Check-up
It’s important to take your child to regular check-ups, even if they’re not sick. Regular check-ups can help keep your child healthy. Check-ups can find and prevent health problems early.
All care is free unless you have Share of Cost when you qualified for Medi-Cal.
Want to learn more about what services Medi-Cal covers for Kids and Teens?
For more information you can visit https://www.dhcs.ca.gov/kidsandteens or call:
- Your Medi-Cal Managed Care Plan
- Phone: The phone number is on your plan ID card and your plan’s website.
- Website: www.dhcs.ca.gov/mmchpd
- Medi-Cal Member Help Line
- Phone: (800) 541-5555 (TDD (800)430-7077)
- Website: www.dhcs.ca.gov/myMedi-Cal
- Mental Health Services
- Phone: (888) 452-8609
- Website: www.dhcs.ca.gov/cmhp
- Alcohol or Drug Use
- Department of Health Care Services (DHCS) Substance Use Resource CenterPhone: (800) 879-2772Hours: 24 hours a day, 7 days a week
- Website: www.dhcs.ca.gov/sud-netrl
You can also read Medi-Cal’s brochures on services for Children and Teens
During the check-up providers will:
- Do a physical exam
- Check their growth and development
- Ask about their family’s health history
- Give recommended shots, when needed
- Talk about dental health and, when needed, give them fluoride supplements and help find a dentist
- Check their hearing and vision
- Ask about their mental health and emotional well-being, and any alcohol or drug use, as well as help them find resources or support
- Discuss important health topics such as sexual health, nutrition, safety, and protecting skin from the sun

Full-breadth Coverage
Everyone who has Medi-Cal, whether Full-Scope or Restricted, or the Medi-Cal Access Program (MCAP) qualifies for the “full breadth” of medically necessary services during both pregnancy and the year after, even if income increases. This eligibility lasts until the end of the month in which the 365th day post pregnancy occurs.
The coverage is the same as Full-Scope Medi-Cal. Immigration status does not matter. It also doesn’t matter how the pregnancy ends. The only exceptions are if the Medi-Cal was Presumptive Eligibility or Minor Consent or if the person moves out of California. For more information visit: https://mcweb.apps.prd.cammis.medi-cal.ca.gov/news/32244 and the Pregnancy Landing Page https://mcweb.apps.prd.cammis.medi-cal.ca.gov/references/pregnancy-landing
Make sure to report the pregnancy or when it ended! In order for this full, extended coverage to show up in the Medi-Cal eligibility system, the county needs to know that the person is pregnant or was pregnant within the past year. So, people with Medi-Cal need to report pregnancy (or its end) to the county as soon as possible. Documentation of the pregnancy is not required, and the county isn’t supposed to ask for it.
It is also important to report to MCAP the birth of the child (here’s how) or other end of pregnancy (FAX 1-888-889-9238, mail to MCAP, P.O. Box 15559, Sacramento, CA 95852-0559, or phone 1-800-433-2611) as soon as possible.
After the report, MCAP-linked newborns get Medi-Cal from the date of birth and continuously for the first year.
For more information see this Maternal and Children Health Access Fact Sheet

Good oral health is linked to long-term overall health and academic opportunity, however, caries–or tooth decay–remain the most common chronic disease among children in the United States, despite being preventable. In California, tooth decay is a significant public health problem, especially for young children. In a recent California study it was shown that by the third grade over 6 in 10 children (61%) have experienced tooth decay and 1 in 5 children (22%) have untreated tooth decay.
You can use your Medi-Cal coverage to help prevent tooth decay and other oral health issues. The Medi-Cal Dental Program covers a variety of dental services such as:
- Diagnostic and preventive dental hygiene (e.g. examinations, x-rays, and teeth cleanings)
- Emergency services for pain control
- Tooth extractions
- Fillings
- Root canal treatments
- Crowns (prefabricated/laboratory)
- Complete and partial dentures
- Orthodontics for children who qualify
- And more!
For more information please visit our Oral Health page.